Patient
Resources

How Scoliosis Affects Your Teenager’s Body: Understanding the Impact
Scoliosis, a condition characterized by an abnormal curvature of the spine, can have a significant impact on a teenager's body and overall well-being. In this...

My Child has Scoliosis: What Now?
The treatment options for scoliosis will depend on the severity of the curvature, the age and physical development of the child, and any associated symptoms....

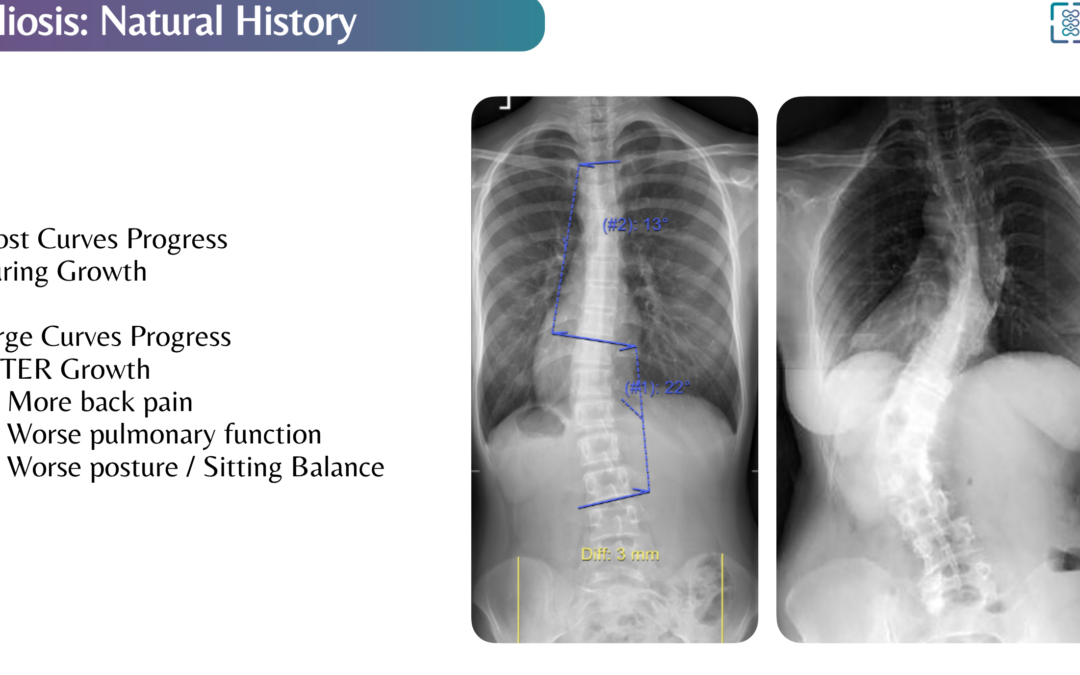
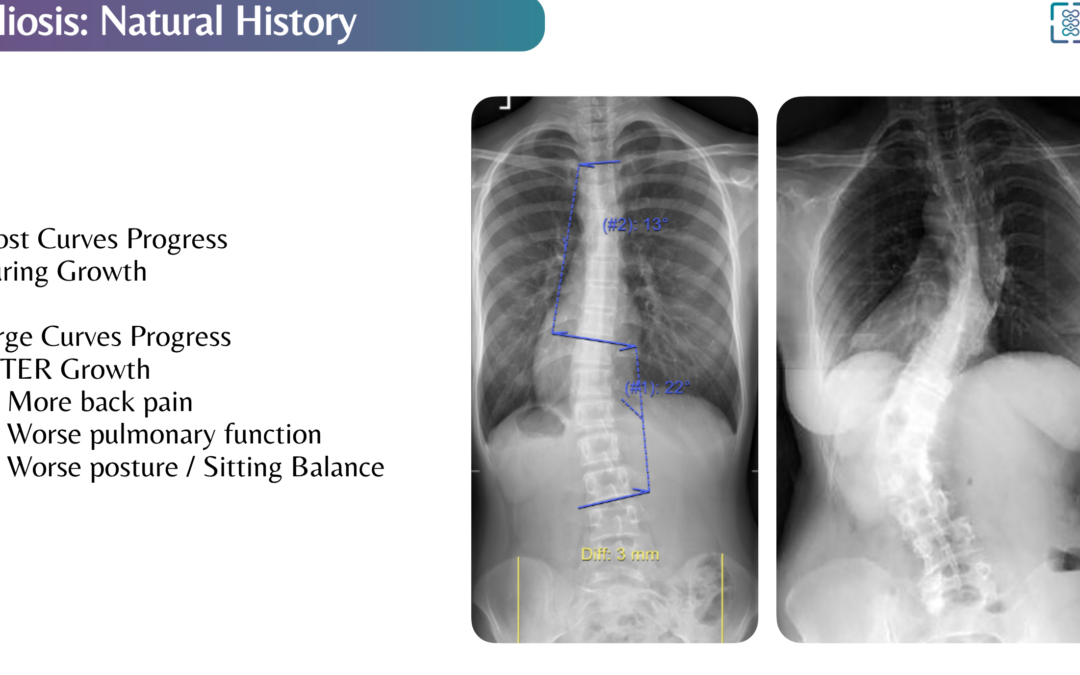
What happens when scoliosis goes untreated?
If scoliosis goes untreated, it can cause the curvature of the spine to worsen over time, leading to more severe symptoms and potentially affecting the...

Effectiveness of Scoliosis Braces: When to Consider Bracing for Your Child
Scoliosis, characterized by an abnormal curvature of the spine, often requires early intervention to prevent progression and manage symptoms. Bracing is a...

How to persuade your teen to comply with scoliosis treatment and how do you help them navigate the most common emotions associated with scoliosis.
Scoliosis, a condition characterized by an abnormal curvature of the spine, requires dedicated treatment and support, particularly when it affects teenagers....

What type of doctor should you see for scoliosis? A list of their pros and cons
Scoliosis is a medical condition involving an abnormal curvature of the spine. There are several healthcare providers and specialists who can be involved in...

Mobile Device-based 3D Scanning Accurately Captures Deformity in Adolescent Idiopathic Scoliosis
Authors Malcolm DeBaun and Dr. John S. Vorhies Abstract/Introduction: Screening and diagnosis in adolescent idiopathic scoliosis (AIS) currently relies on...

Scoliosis Research
The National Scoliosis Clinic is engaged in academic research with our partners to develop peer-reviewed and clinically-proven technology. We are excited to...

The National Scoliosis Clinic Approach
Who is the National Scoliosis Clinic For? The NSC is available for those who want more oversight of their condition by healthcare professionals trained to...

What Are The Treatment Options for Scoliosis
Bracing has historically been the most common option, and is still frequently used in pediatric scoliosis cases where the spinal curve is 20 to 40 degrees....

What happens when scoliosis goes untreated?
If scoliosis goes untreated, it can cause the curvature of the spine to worsen over time, leading to more severe symptoms and potentially affecting the...

Effectiveness of Scoliosis Braces: When to Consider Bracing for Your Child
Scoliosis, characterized by an abnormal curvature of the spine, often requires early intervention to prevent progression and manage symptoms. Bracing is a...

What Are The Treatment Options for Scoliosis
Bracing has historically been the most common option, and is still frequently used in pediatric scoliosis cases where the spinal curve is 20 to 40 degrees....

How Is Scoliosis Diagnosed
Manual The most common adolescent screening method has been to manually assess the curvature of the spine while the patient bends over to touch toes. This...
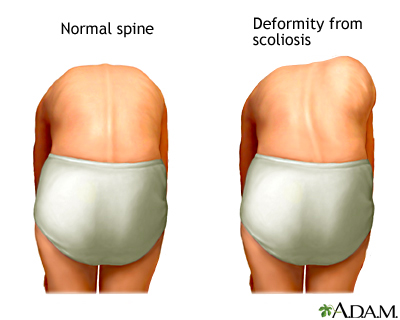
What Is Scoliosis
A healthy human spine is relatively straight when viewed from behind and has a natural S-curve when viewed from the side. A spine with scoliosis bends,...

What happens when scoliosis goes untreated?
If scoliosis goes untreated, it can cause the curvature of the spine to worsen over time, leading to more severe symptoms and potentially affecting the...

How Is Scoliosis Diagnosed
Manual The most common adolescent screening method has been to manually assess the curvature of the spine while the patient bends over to touch toes. This...

Mobile Device-based 3D Scanning Accurately Captures Deformity in Adolescent Idiopathic Scoliosis
Authors Malcolm DeBaun and Dr. John S. Vorhies Abstract/Introduction: Screening and diagnosis in adolescent idiopathic scoliosis (AIS) currently relies on...

Scoliosis Research
The National Scoliosis Clinic is engaged in academic research with our partners to develop peer-reviewed and clinically-proven technology. We are excited to...

How Scoliosis Affects Your Teenager’s Body: Understanding the Impact
Scoliosis, a condition characterized by an abnormal curvature of the spine, can have a significant impact on a teenager's body and overall well-being. In this...

What happens when scoliosis goes untreated?
If scoliosis goes untreated, it can cause the curvature of the spine to worsen over time, leading to more severe symptoms and potentially affecting the...
What Is Scoliosis
A healthy human spine is relatively straight when viewed from behind and has a natural S-curve when viewed from the side. A spine with scoliosis bends,...

My Child has Scoliosis: What Now?
The treatment options for scoliosis will depend on the severity of the curvature, the age and physical development of the child, and any associated symptoms....

Effectiveness of Scoliosis Braces: When to Consider Bracing for Your Child
Scoliosis, characterized by an abnormal curvature of the spine, often requires early intervention to prevent progression and manage symptoms. Bracing is a...

How to persuade your teen to comply with scoliosis treatment and how do you help them navigate the most common emotions associated with scoliosis.
Scoliosis, a condition characterized by an abnormal curvature of the spine, requires dedicated treatment and support, particularly when it affects teenagers....

What type of doctor should you see for scoliosis? A list of their pros and cons
Scoliosis is a medical condition involving an abnormal curvature of the spine. There are several healthcare providers and specialists who can be involved in...

The National Scoliosis Clinic Approach
Who is the National Scoliosis Clinic For? The NSC is available for those who want more oversight of their condition by healthcare professionals trained to...

What Are The Treatment Options for Scoliosis
Bracing has historically been the most common option, and is still frequently used in pediatric scoliosis cases where the spinal curve is 20 to 40 degrees....
Frequently Asked Questions
Patient education and participation in your care plan is a key part of what makes the National Scoliosis Clinic different from traditional scoliosis care models. Explore resources below to learn more about scoliosis, treatment options and NSC.
What do sports physicals cover?
Sports physicals, also known as pre-participation physical evaluations (PPEs), are designed to assess an individual’s overall health and determine whether they are medically cleared to participate in a sport. Sports physicals typically include a thorough medical history review, a physical examination, and any necessary diagnostic tests or screenings.
It is recommended that children and adolescents receive PPEs beginning in middle school (or following recovery from an injury). These should be scheduled at least six weeks before practice begins for their season to allow time for further assessment or treatment if recommended following the PPE.
During a sports physical, the healthcare provider will typically ask about the individual’s medical history, including any past or current injuries, illnesses, or conditions that may affect their ability to participate in sports. They may also ask about medications the individual is taking and any allergies they have.
The physical examination will typically include a measurement of the individual’s height, weight, and vital signs, as well as an assessment of their musculoskeletal system. The healthcare provider may check the individual’s flexibility, strength, and range of motion, and may also check for any signs of abnormalities or injury.
A component of the PPE that parents and guardians may want to inquire about is the assessment of their children’s spine for scoliosis especially if there is a family history of this condition. Adolescent Idiopathic Scoliosis (AIS) is often missed and many schools no longer perform population wide screening for AIS. It is a noninvasive and quick assessment that can be performed in a physician’s office.
In addition to the medical history review and physical examination, the healthcare provider may also recommend certain diagnostic tests or screenings based on the individual’s age, medical history, and type of sport they will be participating in. These may include tests for vision and hearing, electrocardiography (ECG), or other tests as needed.
It is important to remember that sports physicals are not a substitute for a comprehensive medical evaluation. If you have any concerns about your health or the health of your child, it is important to speak with a healthcare provider.
What do school health screenings cover?
School health screenings are designed to identify any potential health issues that may affect a student’s ability to learn and participate in school activities. The specific screenings that are performed will depend on the student’s age and the policies of the school or school district. Screenings may differ by state as well.
In general, school health screenings may include the following:
Vision and hearing screenings: These screenings are designed to identify any vision or hearing problems that may affect a student’s ability to learn.
Height and weight measurements: These measurements are taken to assess the student’s growth and development.
Blood pressure screenings: These screenings are used to check for high blood pressure, which can be a risk factor for heart disease and other health problems.
Scoliosis screenings: These screenings are used to check for abnormal curvature of the spine, which can cause discomfort and other health problems if left untreated.
Pediatric scoliosis screenings are only mandated in 33 states
Screening for scoliosis then falls to the families and primary care caregivers
Dental screenings: These screenings are used to identify any dental problems that may need to be addressed.
Immunization status: Students may be required to show proof of certain immunizations in order to attend school.
It is important to note that school health screenings are not a substitute for a comprehensive medical evaluation. If you have any concerns about your child’s health, it is important to speak with a healthcare provider.
How often is it okay for a child to be x-rayed?
X-rays are a type of medical imaging that uses radiation to produce images of the inside of the body. While x-rays can be useful for diagnosing and monitoring a wide range of medical conditions, they do expose the body to small amounts of radiation. For this reason, it is generally recommended to limit the use of x-rays to situations where they are medically necessary.
The frequency with which a child should be x-rayed will depend on their specific health needs and the recommendations of their healthcare provider. Some children may need to have x-rays more frequently than others, depending on their medical history and the nature of their condition. Pediatric organizations recommend limiting x-rays to no more than every six to twelve months for high-risk children needing monitoring.
Common reasons that your child may require an x-ray:
- Dental exam
- To assess cavities, wisdom teeth, causes of dental pain
- Bone exams
- To screen for fractures, infection, or conditions like scoliosis
- Heart and lung exams
- To assess lung conditions like pneumonia or if suspected damage has occurred to major blood vessels
- Abdominal exam
- To check if your child swallowed a foreign object or is experiencing certain kinds of abdominal pain
It is generally recommended to avoid exposing children to unnecessary radiation, as their bodies are still developing and may be more sensitive to the effects of radiation. However, in some cases, the potential benefits of x-rays may outweigh the potential risks. Your child’s healthcare provider will be able to assess your child’s specific needs and determine if x-rays are necessary in their case.
If your child does need to have an x-ray, it is important to follow the recommendations of their healthcare provider and to discuss any concerns you may have about the procedure. They can provide you with more information about the potential risks and benefits of x-rays and help you to make an informed decision about your child’s care.
I had scoliosis growing up, do I need to have my kids evaluated?
If you had scoliosis growing up, it is possible that your children may be at an increased risk of developing the condition as well. However, it is important to note that scoliosis is a complex condition that is not fully understood, and the exact cause of most cases is unknown. While genetics may play a role in the development of scoliosis, it is not necessarily a direct cause-and-effect relationship.
Risk factors for scoliosis include:
- Age: signs and symptoms usually occur in adolescence
- Sex: girls are at higher risk of developing severe scoliosis
- Family history: scoliosis can run in families but most individuals don’t have a family history of the condition
If you are concerned about your children’s risk of developing scoliosis, it is a good idea to speak with a healthcare provider. They can assess your children’s risk and recommend any necessary screenings or evaluations. It is generally recommended that children be screened for scoliosis as part of routine check-ups, particularly during the ages when scoliosis is most commonly diagnosed (between the ages of 10 and 18).
If your children do not have any signs or symptoms of scoliosis, it is unlikely that they will need any special evaluations or screenings. However, if they do develop scoliosis or any other spinal abnormalities, it is important to seek medical attention as soon as possible to ensure that the condition is properly diagnosed and treated.
What causes back pain in children and adolescents?
Back pain is a common complaint among children and adolescents, and it can have a variety of causes. Most of the time there is no known cause and it is believed to be muscular. Some common causes of back pain include:
- Poor posture: They may develop poor posture habits as a result of activities such as sitting for long periods of time or carrying heavy backpacks. Poor posture can lead to muscle strain and discomfort.
- Musculoskeletal issues: Conditions involving abnormal curvature of the spine like, lordosis, or kyphosis can cause discomfort and other symptoms.
- Injuries: Injuries like sprains and strains can be caused by a variety of factors, including participation in sports, falls, or accidents. Patients may also get stress fractures in their lower back.
- Inflammatory conditions: Conditions like arthritis or ankylosing spondylitis involve inflammation of the joints and spine and can cause discomfort and other symptoms.
- Other medical conditions: Back pain in children and adolescents can also be caused by other medical conditions such as kidney infections, urinary tract infections, or tumors.
If your child or adolescent is experiencing back pain, it is important to speak with a healthcare provider for a proper evaluation and treatment. Make sure to document when your child started experiencing these symptoms, if there is a family history of conditions, and whether your child may have suffered an injury recently. The healthcare provider will be able to determine the cause of the back pain and recommend appropriate treatment options.
What causes leg length discrepancy in kids?
Leg length discrepancy, also known as limb length discrepancy, refers to a condition in which one leg is shorter than the other. Some children are born with congenital limb differences that cause their legs or arms to grow at different rates.
Leg length discrepancy can be caused by a variety of factors, including:
- Congenital conditions: Some children are born with leg length discrepancies due to congenital conditions such as congenital hip dysplasia or congenital short femur. These conditions are present at birth and can affect the development of the legs.
- Growth plate injuries: Growth plate injuries, also known as epiphyseal fractures, can occur when the growth plates (areas of developing bone tissue near the ends of the bones) are damaged. This can cause one leg to grow more slowly than the other, resulting in a leg length discrepancy.
- Infections: Infections, such as osteomyelitis (an infection of the bone) can cause damage to the bones and disrupt normal growth, leading to a leg length discrepancy.
- Neuromuscular conditions: Certain neuromuscular conditions, such as cerebral palsy or spina bifida, can affect the development of the legs and cause a leg length discrepancy.
- Trauma: Trauma to the legs, such as fractures or injuries sustained in a car accident, can also cause a leg length discrepancy.
- Scoliosis: Pediatric scoliosis won’t cause one leg to be anatomically shorter than the other, the abnormal curvature of the spine can cause the pelvis to be uneven and one leg may appear longer than the other. This is an example of Functional Leg Length Discrepancy.
Leg length discrepancies can cause discomfort and other symptoms, such as difficulty walking or standing. Treatment for leg length discrepancies may include the use of shoe inserts, leg braces, or surgery, depending on the severity of the discrepancy and any associated symptoms. It is important to speak with a healthcare provider for a proper evaluation and treatment.
Why don't all schools screen for scoliosis?
Scoliosis is a condition that affects the curvature of the spine and can cause discomfort and other health problems if left untreated. While not a common condition, early diagnosis and treatment of scoliosis can help to prevent it from worsening.
In 2018, the US Preventive Services Task Force (USPSTF) determined that there was insufficient evidence to recommend for or against routine screening for scoliosis. The investigation acknowledged that screening for scoliosis and bracing for scoliosis were effective, but the long-term benefits of these practices did not have sufficient evidence to support these efforts. For this reason, the performance of scoliosis screening will vary depending on the state and the policies of the individual school or school district.
It is important to note, however, that the major specialty societies made up of pediatricians and orthopedic surgeons have independently recommended screening programs for scoliosis. The American Academy of Orthopedic Surgeons (AAOS), the American Academy of Pediatrics (AAP), the Pediatric Orthopedic Society of North America (POSNA), and the Scoliosis Research Society (SRS) all recommend for routine scoliosis screenings at ages 10 & 12 for females, and once at age 13-14 for male children.
If you are concerned about your child’s risk of developing scoliosis or have noticed any signs or symptoms of the condition, it is important to speak with a healthcare provider. They can assess your child’s risk and recommend any necessary screenings or evaluations.
At what age should I be concerned about scoliosis?
Scoliosis is a condition that can occur at any age, but it is most commonly diagnosed in children and adolescents. The majority of cases of pediatric scoliosis are diagnosed in children between the ages of 10 and 18. This is called adolescent idiopathic scoliosis. Other types of scoliosis can be diagnosed at any age. Some spines are curved because the bones are not formed properly (congenital scoliosis) and some can be found even in infants (early onset scoliosis).
It is important for children and adolescents to be regularly screened for scoliosis, as early diagnosis and treatment can help to prevent the condition from worsening. Many schools and pediatrician offices perform scoliosis screenings as part of routine check-ups, although it is also possible to request a screening if you are concerned about your child’s spine.
If you are an adult and you are concerned about scoliosis, it is a good idea to speak with your healthcare provider. They can evaluate your spine and determine if you have scoliosis or any other spine conditions that may be causing discomfort or pain. Treatment options for scoliosis may include physical therapy, bracing, or surgery, depending on the severity of the curvature and any associated symptoms.
Can wearing a heavy backpack cause scoliosis in children?
There is no direct evidence that wearing a heavy backpack can cause scoliosis, a condition in which the child’s spine curvature is abnormally distorted. Scoliosis is generally thought to be caused by a combination of genetic and environmental factors. While carrying a heavy backpack may put additional stress on the spine and muscles, it is unlikely to cause scoliosis on its own.
That being said, carrying a heavy backpack can cause discomfort and muscle strain, particularly if the backpack is not worn correctly. It is important to wear a backpack correctly, with the weight evenly distributed and the straps tightened so that the backpack sits close to the body. This can help to prevent discomfort and muscle strain, as well as poor posture.
If you are experiencing discomfort or pain while carrying a heavy backpack, it is important to address the issue. You may need to adjust the way you are carrying the backpack, or consider using a different type of bag. If you are experiencing ongoing discomfort or pain, it is a good idea to speak with a healthcare provider for further evaluation and treatment.
Here are some tips to reduce the chance of experiencing back pain while wearing a backpack:
- Don’t single strap, double strap
- Wear both straps of the backpack to create an even load; this may be especially important for those with known scoliosis.
- Wear it high and tight, not low and loose
- Ideally the backpack will sit high on the back and be close to the body.
- Keep heavy items close
- Pack heavier items closer to the back to reduce the strain they will create on the back.
- Parents, buy smaller backpacks for your kids!
- The backpack should carry what is needed for their school day only to prevent your child from overloading it with extra items.
- Look for wider padded straps
- These will be more comfortable than narrow thin straps.
- The 10% rule
- A good rule of thumb is that the backpack and its contents should not weigh more than 10% of the child’s bodyweight
When is my child most at risk for developing scoliosis?
Scoliosis is most commonly diagnosed in children and adolescents between the ages of 10 and 18.
Children are most at risk for developing scoliosis or suffering an exacerbation of their scoliosis at the onset of puberty when they will hit a growth spurt. This is why early diagnosis and treatment is important and why most children and adolescents are screened for scoliosis at skill or as part of a check-up with their pediatrician. Parents and guardians should remain vigilant though as not all schools perform scoliosis screenings and oftentimes pediatricians may miss symptoms of scoliosis until they are readily apparent.
It is not entirely clear why some children develop scoliosis and others do not. It is thought that scoliosis may be caused by a combination of genetic and environmental factors. Children with certain genetic conditions, such as Marfan syndrome or Ehlers-Danlos syndrome, may be at an increased risk of developing scoliosis.
What medical conditions might cause scoliosis?
While most of the time there is no known cause of scoliosis, there are several medical conditions that may increase the risk of developing scoliosis or cause scoliosis to worsen. These conditions include:
- Marfan syndrome: Marfan syndrome is a genetic condition that affects the connective tissues in the body.
- Ehlers-Danlos syndrome: Ehlers-Danlos syndrome is a group of genetic disorders that affect the connective tissues in the body.
- Muscular dystrophy: Muscular dystrophy is a group of genetic disorders that affect muscle strength and function.
- Cerebral palsy: Cerebral palsy is a neurological disorder that affects movement and muscle tone.
- Spina bifida: Spina bifida is a birth defect that affects the development of the spinal cord and spine.
- Other genetic conditions.: Patients with a variety of other genetic conditions such as neurofibromatosis, osteogenesis imperfecta, Prader Willi, and a variety of skeletal dysplasias can also be associated with scoliosis.
- Some patients have congenital scoliosis, where the bones of the spine are not formed normally before birth. The abnormal shape of the bones can lead to a curvature of hte spine.
Parents should also take into consideration any family history of scoliosis as their child enters puberty and be aware of the signs and symptoms of scoliosis.
What tests can be done to detect scoliosis?
The most common test for pediatric scoliosis is the Adam’s Forward Bend Test, also known as the Adam’s Test. During this test, the healthcare provider will ask the person to bend forward at the waist while standing, with their arms hanging down and their palms facing their legs. The healthcare provider will look for any abnormal curvature of the spine and will also check for any unevenness in the shoulders or hips.
Other tests that may be used to detect scoliosis include:
- X-rays: X-rays are a type of medical imaging that uses radiation to produce images of the inside of the body. X-rays can be used to visualize the spine and check for any abnormal curvature. Parents and guardians will want to be mindful of how much radiation their child is exposed to over time.
- Magnetic resonance imaging (MRI): MRI is a type of medical imaging that uses magnetic fields and radio waves to produce detailed images of the inside of the body. MRI can be used to visualize the spine and check for any abnormalities.
- Computerized tomography (CT) scan: A CT scan is a type of medical imaging that uses X-rays and computer technology to produce detailed cross-sectional images of the inside of the body. CT scans can be used to visualize the spine and check for any abnormalities.
It is important to speak with a healthcare provider if you are concerned about scoliosis or have noticed any signs or symptoms of scoliosis. They can recommend the appropriate tests and evaluations to diagnose and monitor the condition.
How can I check my child for scoliosis?
There are several steps you can take to check your child’s spine for scoliosis:
- Look for visible signs of scoliosis: Some signs of scoliosis to look for include uneven shoulders, a visible curvature of the spine, or uneven hips.
- Perform the Adam’s Forward Bend Test: This test involves asking your child to bend forward at the waist while standing, with their arms hanging down and hands overlapped so they are at the same level. Look for any abnormal curvature of the spine and any unevenness in the shoulders or hips.
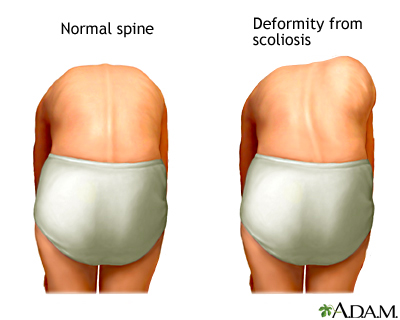
- Consult a healthcare provider: If you have any concerns about your child’s spine or if you notice any signs or symptoms of scoliosis, it is important to speak with a healthcare provider. They can perform a thorough evaluation and recommend any necessary tests or treatments.
It is important to note that self-examination is not a substitute for a professional evaluation. If you are concerned about your child’s risk of developing scoliosis or have noticed any signs or symptoms of the condition, it is important to speak with a healthcare provider or scoliosis specialist for a proper evaluation and treatment.
What happens when scoliosis goes untreated?
If scoliosis goes untreated, it can cause the curvature of the spine to worsen over time, leading to more severe symptoms and potentially affecting the person’s ability to perform daily activities.
Untreated scoliosis can cause a variety of symptoms, including:
- Back pain: Scoliosis can cause discomfort and pain in the back, particularly if the curvature is severe.
- Nerve pain- Untreated severe scoliosis can cause a pinching of the nerves which would be felt as pain in the legs or difficulty walking long distances.
- Difficulty breathing: In severe cases, scoliosis can cause the ribs to press against the lungs and restrict breathing.
- Uneven shoulders or hips: Scoliosis can cause the shoulders or hips to appear uneven, as the spine is not straight.
- Posture problems: Scoliosis can cause poor posture, as the person may lean to one side to compensate for the curvature of the spine.
It can also lead to other complications such as arthritis, joint problems, and decreased mobility. Treatment for scoliosis may include physical therapy, bracing, or surgery, depending on the severity of the curvature and any associated symptoms. It is important to speak with a healthcare provider if you are concerned about scoliosis or have noticed any signs or symptoms of the condition.
Can genetic testing detect scoliosis?
Genetic testing can be used to identify genetic changes or mutations that may be associated with an increased risk of developing certain conditions. However, it is important to note that genetic testing is not a perfect predictor of an individual’s risk of developing a specific condition, and the results of genetic testing can be complex and difficult to interpret.
Important risk factors to consider for scoliosis are age and sex. Adolescents (10-18 years old) are most likely to develop Adolescent Idiopathic Scoliosis (AIS) which is the most common form affecting children while Adult Scoliosis is typically only present in those aged 60 and older. While boys and girls have similar risk of developing mild AIS, girls are more likely to have spinal curvature progress to moderate and severe stages when intervention is necessary.
If you are interested in genetic testing to assess your risk of developing scoliosis or to determine if you have a genetic condition that may increase your risk of scoliosis, it is important to speak with a healthcare provider. Previous attempts to commercialize genetic testing for scoliosis failed as they offered no predictive value and were not consistent across different races. They can provide you with more information about the potential risks and benefits of genetic testing and help you to make an informed decision about whether genetic testing is right for you.
How often should kids be checked for scoliosis?
It is generally recommended that children be screened for scoliosis as part of routine check-ups, particularly during the ages when scoliosis is most commonly diagnosed (between the ages of 10 and 18). It is important to detect scoliosis as early as possible, as early diagnosis and treatment can help to prevent the condition from worsening.
If your child does not have any signs or symptoms of scoliosis and does not have any underlying medical conditions that increase their risk of developing the condition, it is unlikely that they will need to be screened for scoliosis more frequently than during routine check-ups. Many children may be screened at their schools if they are in a state or district that include scoliosis as a part of their health screenings. However, if your child does have any signs or symptoms of scoliosis or if you are concerned about their risk of developing the condition, it is a good idea to speak with a healthcare provider. They can assess your child’s risk and recommend how often screenings and evaluations should occur.
My child has scoliosis: What now?
The treatment options for scoliosis will depend on the severity of the curvature, the age and physical development of the child, and any associated symptoms.
An important data point to know following your child’s diagnosis:
- What is the Cobb Angle of my child’s spine? This is the measure of how severe the curvature of the spine is.
- Less than 20°
- This is considered Low Risk of developing severe scoliosis; your child can be monitored with follow up assessment.
- Between 20° and 25°
- This is considered Moderate Risk of developing severe scoliosis. If your child has significant growth remaining they may benefit from undergoing some form of treatment
- Greater than 25°
- This is considered High Risk. It is advisable for you to consult with a scoliosis specialist to determine the appropriate treatment for your child.
- Less than 20°
Possible treatment options for scoliosis include:
- Observation: In some cases, mild scoliosis may not require treatment and may be monitored over time to see if the curvature worsens.
- Physical therapy: Physical therapy can help to strengthen the muscles around the spine and improve flexibility, which can help to alleviate discomfort and improve mobility.
- Bracing: If the curvature of the spine is moderate and there is growth remaining, a brace may be recommended to help slow the progression of the scoliosis. Braces can help to realign the spine and prevent the curvature from worsening.
- Surgery: In severe cases of scoliosis, surgery may be recommended to correct the curvature of the spine. There are several types of scoliosis surgery, and the specific type of surgery that is recommended will depend on the severity of the curvature and the age and physical development of the child.
It is important to work with a healthcare provider to determine the best course of treatment for your child’s scoliosis. They can provide you with more information about the potential risks and benefits of different treatment options and help you to make an informed decision about the best course of action.
What happened with the ScoliScore DNA test?
The ScoliScore DNA test was a genetic test that was developed to assess an individual’s risk of developing adolescent idiopathic scoliosis (AIS), a type of scoliosis that occurs in adolescents (10-18 years old) and has no known cause. The ScoliScore DNA test was designed to analyze a panel of genetic markers associated with the risk of developing AIS and provide a personalized risk assessment based on the results.
The ScoliScore DNA test was developed and marketed by the company Axial Biotech, but it is no longer available. While the ScoliScore DNA test could identify genes that were linked to AIS it’s predictive value was poor and not useful in preventing the onset or early detection of AIS.
It is important to note that while genetic testing can be a useful tool for identifying genetic changes or mutations associated with an increased risk of developing certain conditions, it is not a perfect predictor of an individual’s risk of developing a specific condition. The results of genetic testing can be complex and difficult to interpret, and it is important to speak with a healthcare provider about the potential risks and benefits of genetic testing before making a decision about whether to undergo testing.
What are the different treatments that exist for pediatric scoliosis? How do I pick from them?
Scoliosis is a condition in which the spine is curved instead of straight. Treatment options for scoliosis vary based on the severity of the curve, the age and overall health of the patient, and other factors. Here are some common treatment options for scoliosis:
- Observation: For mild cases of scoliosis, a healthcare professional may recommend simply monitoring the condition over time to see if it progresses. This may involve periodic check-ups and x-rays to track the curvature of the spine.
- Bracing: For children with moderate to severe scoliosis, a back brace may be recommended to help stop the curve from getting worse while the patient finishes growth. The brace is worn for a set number of hours per day and is typically removed for activities such as bathing and exercising. Bracing can typically be stopped once a patient stops growing.
- Physical therapy: Physical therapy (PT) may be recommended to help improve posture and strengthen the muscles in the back and core. This can help with discomfort from scoliosis or other spine conditions. Scoliosis-specific PT is offered by many therapists with the hope it can limit the progression of scoliosis, though the evidence for this result is mixed. PT should not be relied on instead of bracing, but it may be used in addition to bracing.
- Surgery: In severe cases of scoliosis, surgery may be recommended to correct the curvature of the spine. This can involve the use of rods, screws, and other hardware to straighten the spine and hold it in place.
When considering treatment options for scoliosis, it is important to consult with a healthcare professional who is a pediatric spine specialist, such as an orthopedic surgeon or neurosurgeon. They will be able to evaluate your specific case and recommend the best treatment plan based on your needs.
Is it better for my child to do PT or have surgery for their scoliosis?
Treatment for pediatric scoliosis depends on the severity of the curvature of your child’s spine and the age of the child. In general, treatment options for scoliosis include physical therapy, bracing, and surgery. The most appropriate treatment option will depend on the specific characteristics of the curve and the overall health of the child.
Physical therapy can be effective in helping to improve flexibility and strength in the muscles around the spine, which can help to alleviate pain and improve mobility. Physical therapy is usually recommended for mild scoliosis or as a supplement to other treatments. The Schroth Method is an exercise program that is a well known form of physical therapy specifically designed to treat scoliosis. This course of treatment can last up to 20 sessions but patients benefit from continuing the program throughout their lifetime.This program is best for small and flexible scoliosis curves.
Bracing is often recommended for children who have a curvature of the spine between 25 and 40 degrees and are still growing. The goal of bracing is to prevent the curve from getting worse and to help the spine grow straight. Oftentimes bracing and physical therapy are the first treatment options to address patients with moderate scoliosis curvature Cobb Angle of 20 – 25 degrees.
Surgery may be recommended for severe cases of scoliosis that are not responding to other treatments or for children who have stopped growing and have a curvature of the spine greater than 45 degrees. The goal of surgery is to straighten the spine and to improve the overall appearance and function of the back.
It is important to discuss all treatment options with a healthcare professional who is familiar with your child’s specific case. They will be able to provide you with more detailed information about the benefits and risks of each treatment option and help you to make an informed decision about the best course of action for your child.
Video Library
Patient Journey: Watch Lisa H’s Story
Provider Insights: Meet Alison Dyszel